



Quick Links:






What is heat stress?
Heat stress can be defined as the net heat load to which a person is exposed from the combined contributions of metabolic heat, environmental factors, and clothing worn which results in an increase in heat storage in the body. The neat heat load on the body is the total heat stress which is considered to be the sum of the heat generated in the body (metabolic heat), plus the heat gained from the environment (environmental heat), minus the heat lost from the body to the environment.
The net heat stress that a person experiences is dependent on a combination of factors such as the climatic conditions, the work environment, demands of the work and personal characteristics. A person experiences a physiological response to the heat load (external or internal), in which the body attempts to increase heat loss to the environment in order to maintain a stable body temperature.
What are the adverse effects of heat stress?
Heat stress becomes a deep concern and a critical hazard when the body becomes overwhelmed and is unable to keep up the rate of heat discharge to the environment that is required in order to maintain a stable body temperature that is vital for normal body functioning.
At some level of heat stress, a person’s compensatory mechanisms are no longer capable of maintaining body temperature at a level required for normal body functioning. As a result, the risk of heat-related illnesses, disorders, and other hazards increases. The level of heat stress at which excessive heat strain will result depends on the heat tolerance capabilities of the worker. However, even though there is a wide range of heat tolerance between workers, each worker has an upper limit for heat stress, beyond which the resulting heat strain can cause the person to become a heat casualty.
Heat illnesses that can be experienced as a result of uncontrolled heat stress include heat stroke, heat exhaustion, heat cramps, heat rash and fainting.
When do employees experience heat stress health effects?
Heat stress can be experienced at any instance and is not only restricted to the summer months and outdoor work alone. Doing strenuous work that has a high metabolic rate wearing high insulating clothing can also contribute significantly to high levels of heat stress. Similarly working in indoor environments where the ambient temperature is elevated because of the operation of heat producing equipment and systems also contribute to high heat stress levels. Furthermore, there are personal factors such as obesity, intake of caffeine and other general health characteristics that make a person more vulnerable to heat stress.
At some level of heat stress, a worker’s compensatory mechanisms are no longer capable of maintaining body temperature at a level required for normal body functions. As a result, the risk of heat-related illnesses, disorders, and other hazards increases. The level of heat stress at which excessive heat strain will result depends on the heat tolerance capabilities of the worker. However, even though there is a wide range of heat tolerance between workers, each worker has an upper limit for heat stress, beyond which the resulting heat strain can cause the worker to become a heat casualty.
How can heat stress be monitored?
Monitoring physiological response of employees is the optimal way to identify heat stress scenarios. Never ignore heat stress symptoms even if the measured environmental parameter is below the limit of the standard referenced. Proactively heat stress can be managed by monitoring the heat index of the environment in which work is being undertaken.
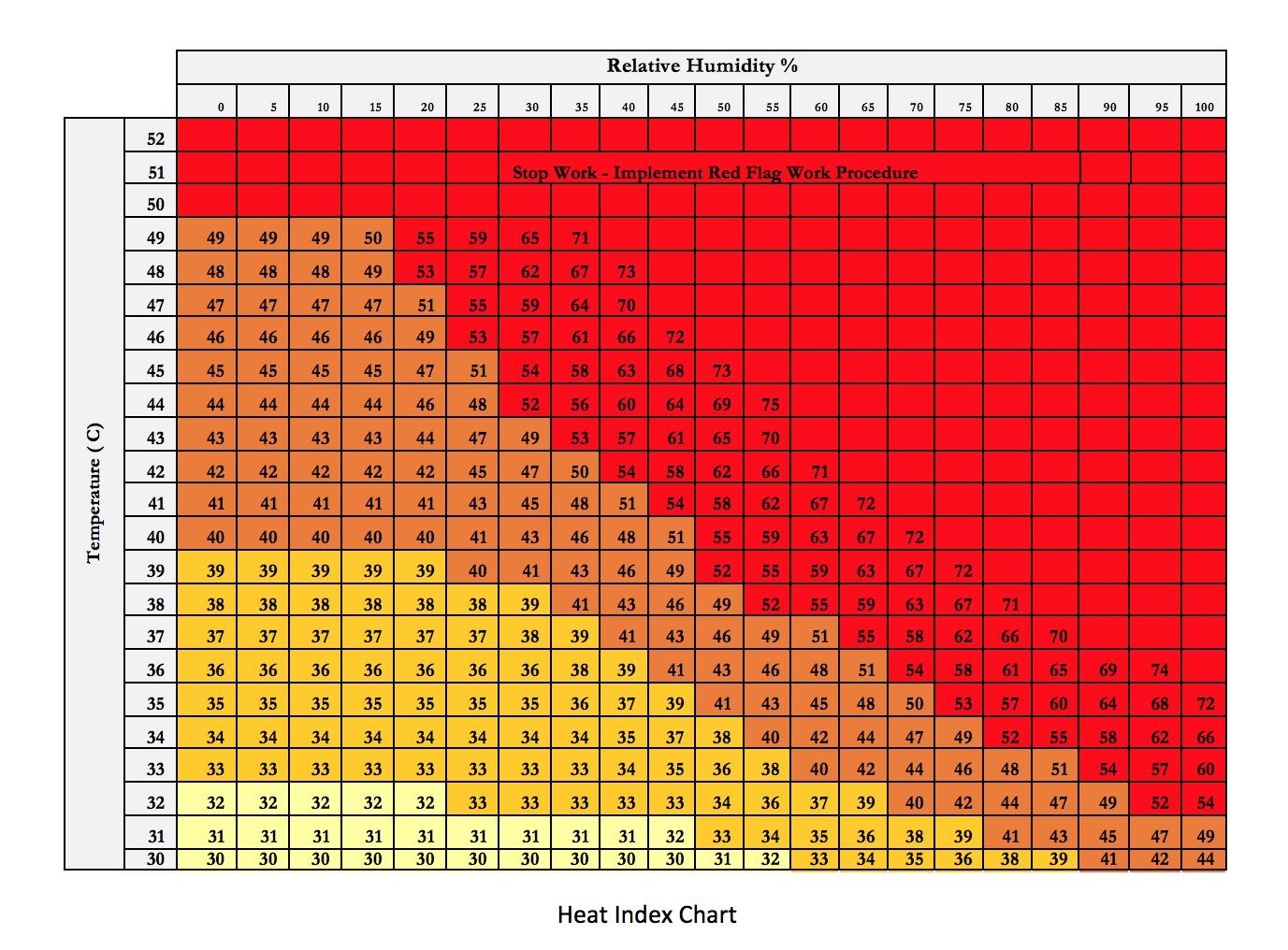
The heat index (HI) is a metric that combines temperature and humidity values to provide an apparent temperature. It is an approximate indication of how hot someone feels. This is a simplified evaluation method and affords good protection against adverse effects of elevated heat stress levels. For a given temperature the higher the humidity the higher the heat index. Higher humidity levels reduce the efficiency of evaporative cooling thereby reducing the rate of excess heat dissipation thereby making an individual feel warmer.
The heat index combines two measured parameters namely the atmospheric temperature and relative humidity. The two obtained values can be combined using the Chart provided below to ascertain the heat index value. The index indicates the temperature that the human body feels. When the index gives a higher temperature, the risk of sustaining heat related illnesses and other injuries increases.
What proactive actions can be taken to prevent heat illnesses?
A combination of both general and job specific controls need to be adopted to manage the risk of heat stress. Recommended actions are based on the measured heat index value. The table below provides recommended resting time and water intake for a given heat index range.
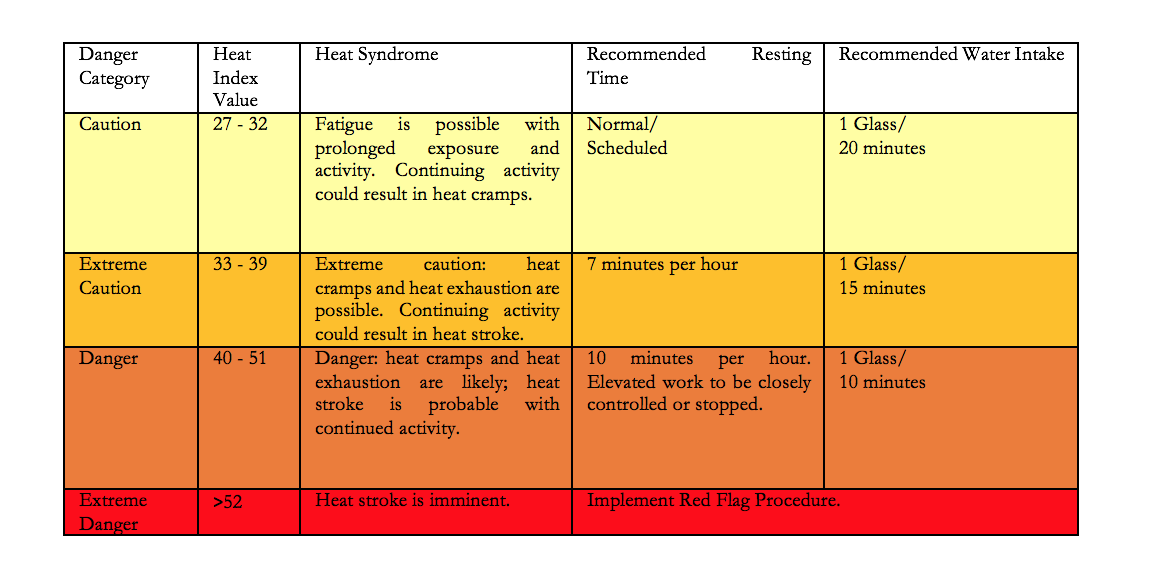
Note! 1 Glass = 250 ml. DO NOT drink more than 1.5 liters per hour (maximum water absorption rate of body)
Apart from this it is the employer’s responsibility to ensure that adequate job specific engineering and administrative controls are in place to ensure that heat stress situations are avoided. Common engineering and administrative measures are provided below.
Red Flag Measures
What job specific engineering controls can be adopted to prevent heat stress?
A range of engineering controls can be adopted to reduce the heat index of the working environment
What job specific administrative controls can be adopted to prevent heat stress?
Scheduling
If possible, perform potentially hot jobs when heat illness conditions are at their minimum. Allow latent heat in equipment to dissipate before work begins. When practical, schedule work for the cooler part of the day, and schedule routine maintenance and repair work in hot areas for the cooler seasons of the year.
Fluid Replacement
Place ample supplies of cooled drinking water in hygienic conditions close to the work area. Because the normal thirst mechanism does not ensure sufficient fluid intake, encourage workers to drink small amounts on a frequent basis.
Acclimatization
Most people get used to heat exposure up to a point. This is called acclimatization and it results in less cardiovascular demand for a given activity. The employee will sweat more efficiently (increasing evaporative cooling) and may lose less salt, thus will more easily maintain normal body temperature. Acclimatization decreases the risk of heat-related illnesses and associated unsafe acts. Deliberate acclimatization involves exposing employees to work in a hot environment for progressively longer periods.
For new workers who will be similarly exposed, the regime should be 20% on day one, with a 20% increase in exposure each additional day
Training
All employees who have the potential to be exposed to elevated levels of heat stress have to be trained periodically. It will be the Department Manager’s responsibility to ensure that appropriate training is imparted. The key topics that will have to be covered include basic understanding of the body’s physiological response to heat stress, signs and symptoms of heat stress and actions that need to be taken to avert adverse consequences of heat stress.
Other Administrative Controls
Reduce the physical demands of work such as excessive lifting or digging by using powered equipment, increase the number of workers assigned to a task, use relief workers, and limit worker occupancy in confined areas.
What specific PPE’s can be used to manage heat stress?
Personal protective equipment is not a substitute for engineering and administrative controls should not be the sole control measure to protect employees from heat stress, however sometimes PPE is required to supplement engineering controls and good work practices. Some of the PPE available include:
Additional recommendations for school sports
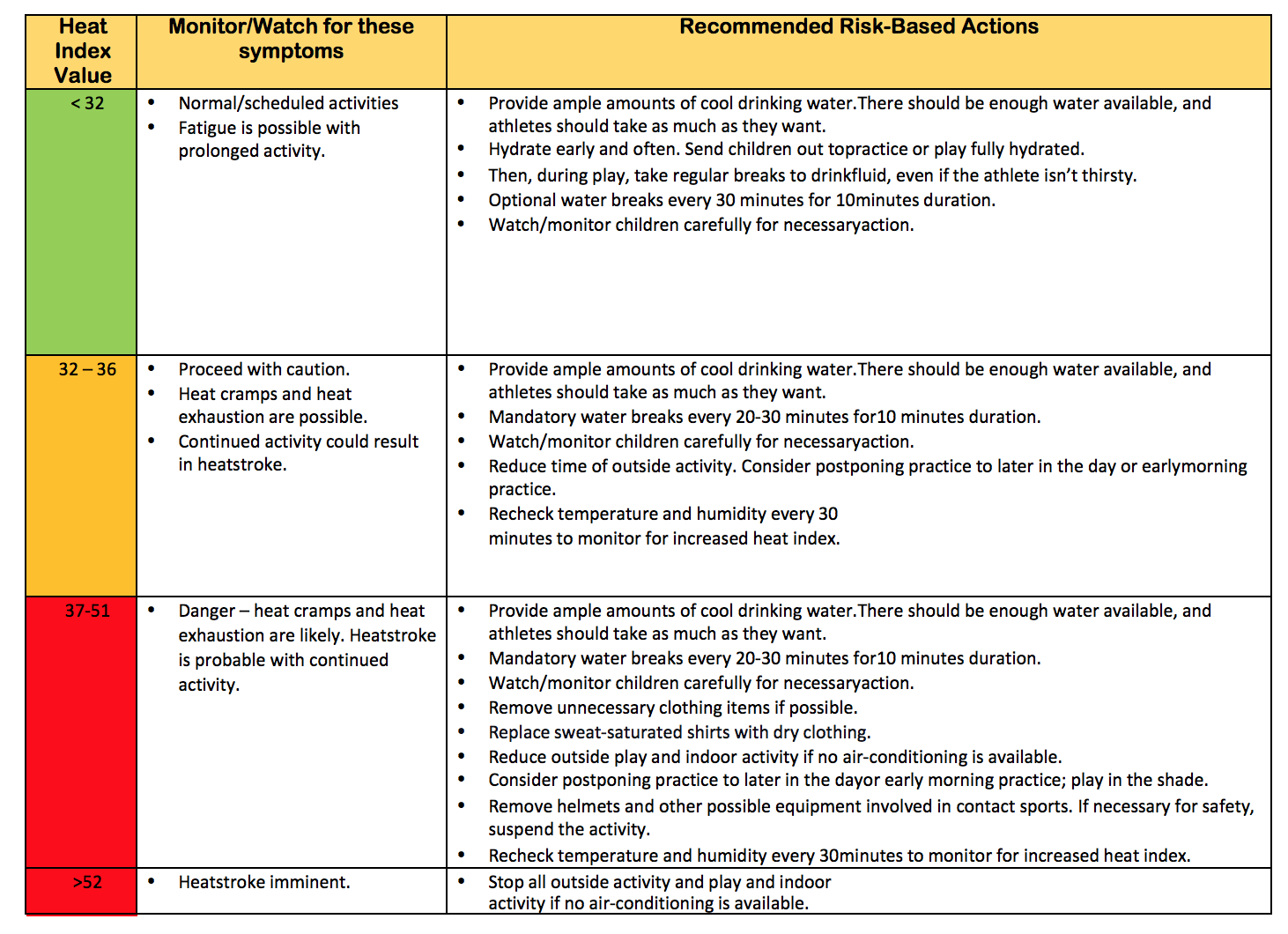
Recommended risk-based actions for school children based on measured Heat Index value
A person’s body temperament, disposition and general health aspects has a great influence on heat stress. Age, weight, degree of physical fitness, acclimatization, metabolism, and a variety of medical conditions such as hypertension all affects an individual’s sensitivity to heat. Even the type of clothing worn must be considered. Prior heat injuries predispose an individual to additional injury.
Certain medical and personal conditions are risk factors for experiencing heat-related illnesses or disorders:
When workers are exposed to hot work environments, they readily show signs of distress and discomfort, such as increased core temperatures and heart rates, headache or nausea, and other symptoms of heat exhaustion. Acclimatization refers to a set of adaptive physiological and psychological adjustments that occur when an individual accustomed to working in a temperate environment undertakes work in a hot or cold environment. These progressive adjustments occur over periods of increasing duration and reduce the strain experienced on initial exposure. This enhanced tolerance allows a person to work effectively under conditions that might have been unendurable before acclimatization.
In heat acclimatization the human body adaptations include:
Metabolic heat generated by the body is an important constituent in the overall heat balance equation of the body. The risk of heat stress increases if the activity is more strenuous and physically demanding. The metabolic heat generated by the body increases as we undertake activities that are more physically demanding.
It should be understood that the limits prescribed by any standard is only indicative in nature. Being below the limit does not guarantee safety. Heat strain experienced by various people vary and is dependent on various factors that are subjective in nature. Monitoring physiological response of employees is the optimal way to identify heat stress scenarios. Never ignore heat stress symptoms even if the measured environmental parameter is below the limit of the standard referenced. Additionally, limits that are stipulated by any standard is for adequately hydrated, unmedicated, healthy workers.
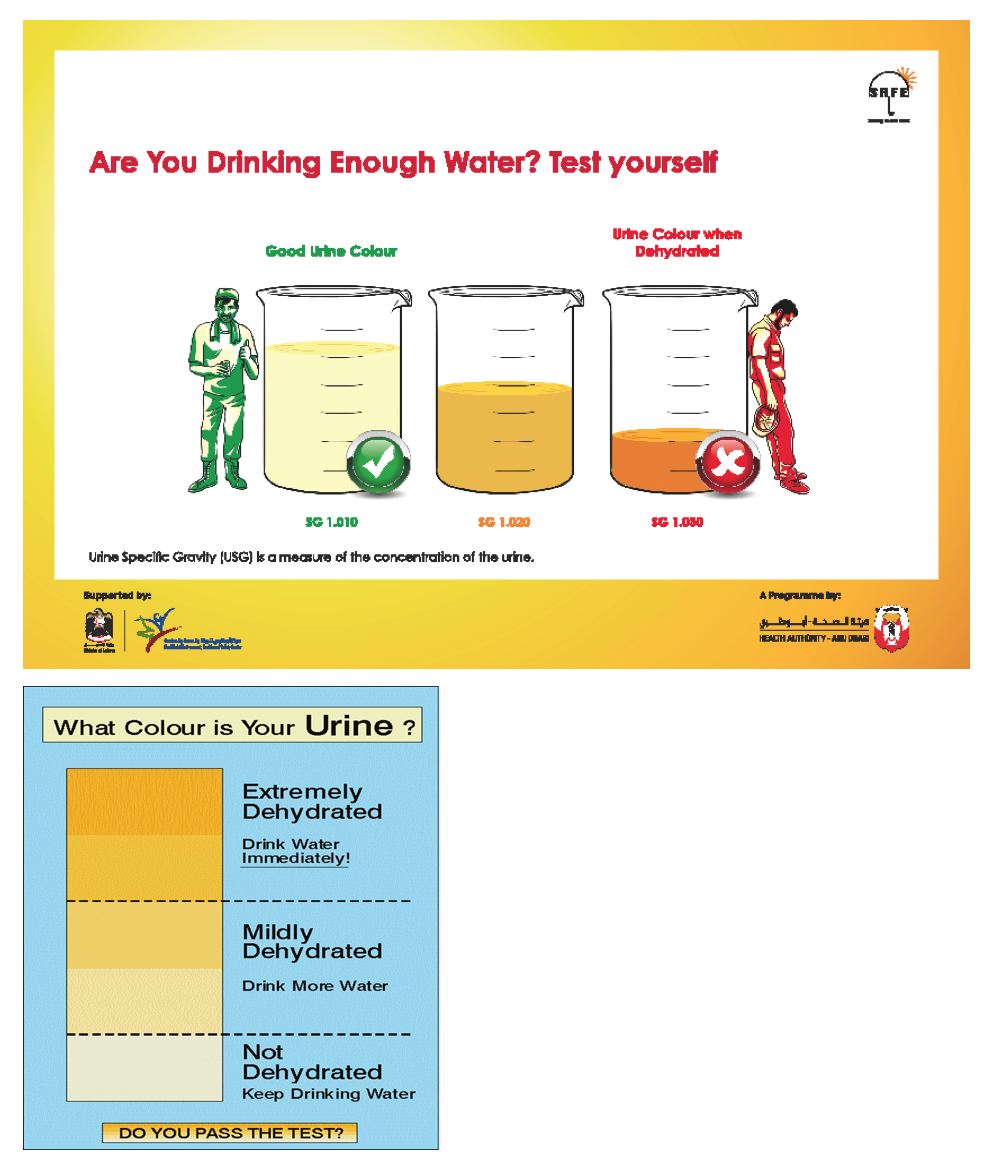
Ensure ample intake of fluids, preferably water, throughout the day, and steer clear of dehydrating beverages like caffeinated drinks. Being hydrated when you start work makes it easier to stay hydrated through the day. If you are dehydrated when you start work, you may not be able to drink enough to catch up with your body’s need for water. Drink before feeling thirsty. By the time you feel thirsty, you are already behind in fluid replacement. Dehydration is a primary contributor to heat exhaustion. Drinking at shorter intervals is more effective than drinking large amounts infrequently.
Do not drink more than 1.5 liters per hour. Drinking too much water or other fluids (sports drinks, energy drinks, etc.) can cause a medical emergency because the concentration of salt in the blood becomes too low.
Some energy drinks contain much more caffeine than standard servings of coffee, tea, or soft drinks. Drinking several energy drinks per day can raise your caffeine levels enough to affect your heart. High caffeine levels can be risky when added to the strain placed on your body by heat